Treatment
Protecting the Heart
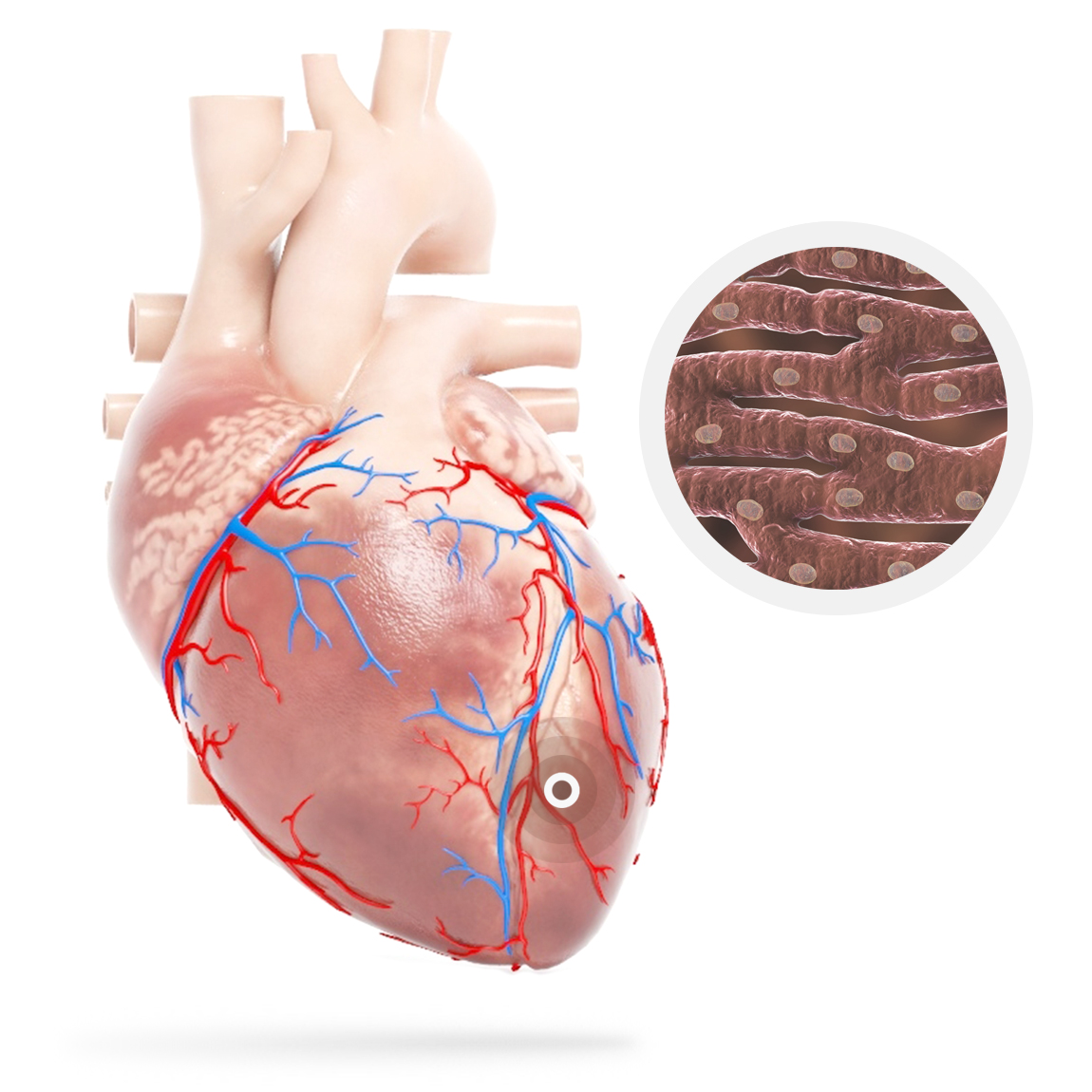
Stress lasting more than approx. 30 mins causes death of the cells and lasting damage whereas reversal of ischemia within this period preserves cellular function.
In the US the median time from MI symptoms to treatment (usually Percutaneous Coronary Intervention (PCI) or “stent”) is 185 mins, meaning most patients experience inevitable irreversible damage, with damage increasing in those patients with delayed time to PCI.



It is estimated that as much as 1.7% of the World’s population are living with Ischaemic heart disease, with a high risk of MI resulting in death or progression to heart failure; described by patients as
Cardiac functional reserve is the difference between peak (i.e. maximal stress at peak exercise) and baseline resting values. With increasing age, natural attrition results in progressive diminution in the pumping capability of the heart and cardiac reserve, while baseline resting cardiac function (dashed horizontal line) remains largely unchanged.
With discrete incidences of cardiomyocyte loss through myocardial infarctions pumping capability plummets stepwise with each incident. When this falls below the normal baseline level, a state of extreme cardiac failure (cardiogenic shock) ensues, which is rapidly followed by death unless drastic measures (e.g. surgery) are successful.
The accelerated deterioration of cardiac pumping capability (secondary to putative myocyte attrition) can be ameliorated with neurohumoral therapies.